Browse by category

CBT for IBS & Gut Microbiome Improvement: Research Brief
CBT for IBS associated with Gastrointestinal Symptom Improvement
Microbiome 9, 236 (2021)
IBS affects 10%-25% of the population worldwide both in bowel symptoms and mental health¹. It affects women 1.5-3x as often as men, and patients report decreased quality of life¹. The bidirectional signaling between brain and the digestion tract may indicate that one affects the other.
This study shows CBT tools such as muscle relaxation, worry control, flexible problem solving, patient education, self-monitoring, and relapse prevention help decrease IBS symptoms, such as abdominal pain, and bowel symptoms, not only by influencing the patient's mental status, but also contributing to healthy gut bacteria.
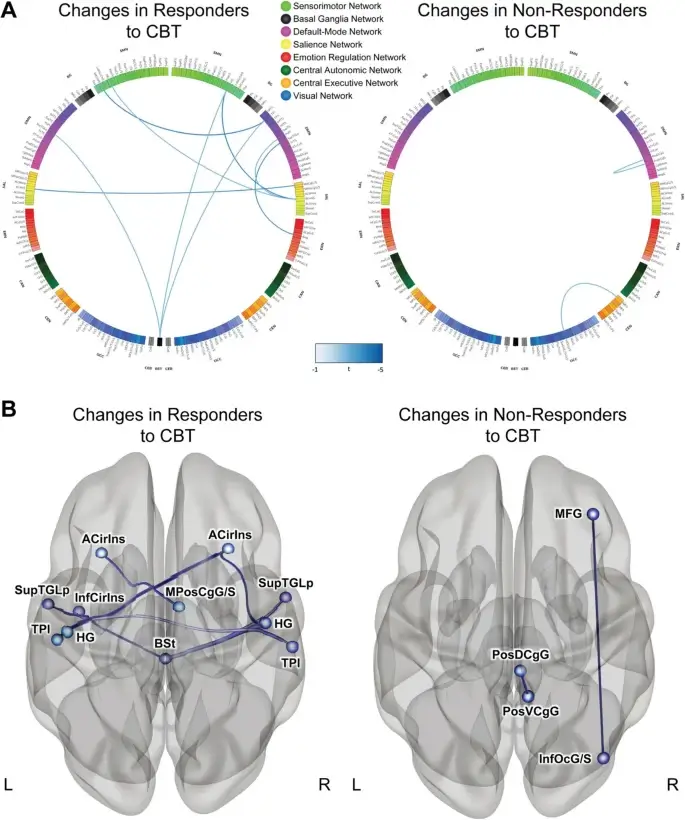
These findings suggest that CBT, among other things, can help reduce functional connectivity in the brain which may turn off, or limit, the positive feedback loop whereby symptoms exacerbate themselves. Brain changes were shown to correlate with microbiome shifts, thus the brain-gut connection is looking more and more substantiated.
Highlights from the Study
“CBT is an effective brain-targeted intervention that teaches information processing skills to address psychological factors known to exacerbate abdominal symptoms including maladaptive coping, intense worry….”
“...responders showed highly significant improvements in several clinical parameters, including IBS symptom severity and its constituent processes (abdominal pain, life satisfaction, bowel dissatisfaction). These clinical improvements were accompanied by functional and structural brain changes...”
“This study demonstrates for the first time that a brief non-drug, non-dietary intervention that teaches information processing skills can modulate key components of the brain-gut-microbiome axis in IBS patients.”
At Feeling Good Institute, we use the various CBT tools and procedures listed as effective for IBS including patient education, self-monitoring, worry control, relapse prevention, and more.
Learn about the essential skills for effective cognitive behavior therapy and how we set therapists up for success.
¹Citation: prevalence of IBS: Canavan, C., West, J., & Card, T. (2014, February 4). The epidemiology of Irritable Bowel Syndrome. Clinical epidemiology. Retrieved May 26, 2022, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3921083/
²Citation primary study: Jacobs, J. P., Gupta, A., Bhatt, R. R., Brawer, J., Gao, K., Tillisch, K., Lagishetty, V., Firth, R., Gudleski, G. D., Ellingson, B. M., Labus, J. S., Naliboff, B. D., Lackner, J. M., & Mayer, E. A. (2021, November 30). Cognitive behavioral therapy for irritable bowel syndrome induces bidirectional alterations in the brain-gut-microbiome axis associated with gastrointestinal symptom improvement - microbiome. BioMed Central. Retrieved May 18, 2022, from https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-021-01188-6